All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The lym Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lym Hub cannot guarantee the accuracy of translated content. The lym and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lymphoma & CLL Hub is an independent medical education platform, sponsored by AbbVie, BeOne Medicines, Johnson & Johnson, Miltenyi Biomedicine, Nurix Therapeutics, Roche, Sobi, and Thermo Fisher Scientific and supported through educational grants from Bristol Myers Squibb, Lilly, and Pfizer. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lymphoma & CLL content recommended for you
Acalabrutinib for untreated CLL: delving into ELEVATE TN phase III trial results
The main results from the ELEVATE TN trial (NCT02475681) in patients with untreated chronic lymphocytic leukemia (CLL) were first presented by Jeff P. Sharman et al. at the 61st ASH Annual Meeting in December 2019. The Lymphoma Hub summary can be found here.
Study design and results
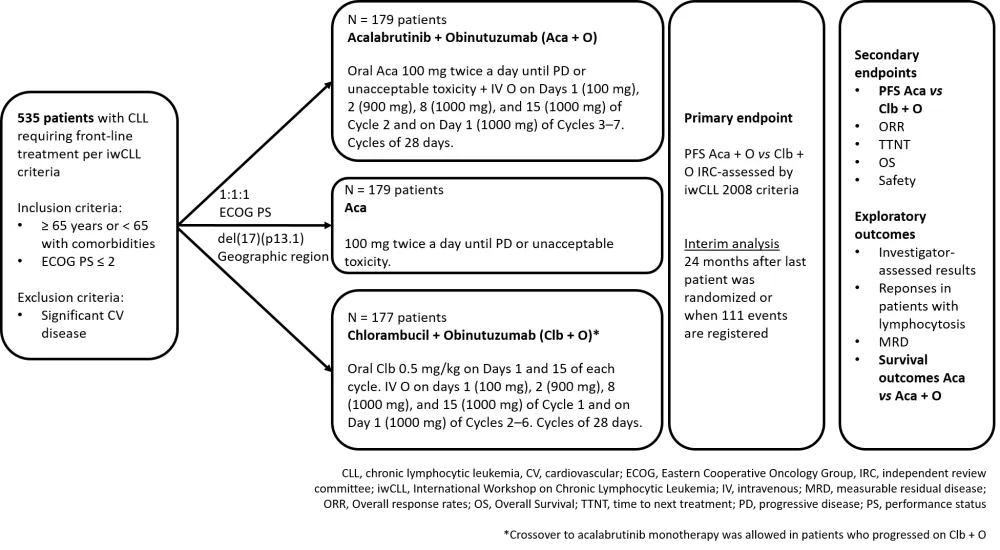
This multicenter, open-label phase III study randomized 535 patients with treatment-naïve CLL to receive acalabrutinib combined with obinutuzumab (Aca + O), acalabrutinib alone (Aca), or chlorambucil with obinutuzumab (Clb + O) (Figure 1). After a median follow-up of 28.3 months, the primary endpoint was met since the Aca + O arm presented a significantly longer progression-free survival (PFS; PFS not reached) compared with the control arm Clb + O (PFS, 22.6 months). This result translated into a 90% reduction in relative risk of progression or death with Aca + O (HR 0.10, 0.06–0.17, p < 0.0001), and led to the approval of acalabrutinib by the U.S. Food and Drug Administration (FDA) for first-line treatment of patients with CLL, alone or in combination with obinutuzumab.
Recently Jeff P. Sharman et al. published in Lancet the full interim analysis,1 giving more detailed information about patient characteristics and secondary analyses. This article focusses on the additional data reported in the publication.
Figure 1. Study design.
Patient's baseline demographic and clinic characteristics were equally distributed between treatment groups. The median age was 70 years, 84% of the patients aged 65 years or older. Performance status (PS) was 0–1 in the vast majority (> 90%) of patients, although almost half of the patients presented with cytopenia at study entry. In the Aca + O, Aca, and Clb + O arms, 64.2%, 74.9%, and 67.2% of the patients, respectively, had a CLL-international prognostic index (CLL-IPI) score between 4–6, considered as high risk. Other high-risk features such as unmutated immunoglobulin heavy-chain variable gene (IGHV), mutated TP53, del(17)(p13.1), or del(11)(q22.3), were determined in a central lab at baseline to be able to analyze the survival outcomes afterward according to these subgroups.
The PFS subgroup analyses HR values for Aca + O vs Clb + O, and Aca vs Clb + O are reported in Table 1. There was a consistent benefit across subgroups in favor of acalabrutinib-containing regimes, which translated into a higher PFS rate at 24 months (Aca + O vs Clb + O) even in patients presenting bulky disease (90% vs 28%), del(11)(q22.3) (87% vs 24%), or unmutated IGHV (91% vs 31%).
Table 1. Prespecified subgroup analyses of PFS for Aca + O vs Clb + O, and Aca vs Clb + O.
|
Aca, acalabrutinib; Clb, chlorambucil; del, deletion; ECOG, Eastern Cooperative Oncology Group; IGHV, heavy-chain variable gene; O, obinutuzumab In bold, subgroups for which a clear benefit cannot be confirmed. |
||
|
HR (95% CI) |
||
|---|---|---|
|
Selected subgroups |
Aca + O vs Clb + O |
Aca vs Clb + O |
|
Overall |
0.1 (0.06–0.17) |
0.2 (0.13–0.30) |
|
Age |
|
|
|
< 65 |
0.02 (0.00–0.17) |
0.19 (0.07–0.52) |
|
≥ 65 |
0.13 (0.07–0.23) |
0.2 (0.12–0.32) |
|
ECOG PS |
||
|
0-1 |
0.09 (0.05–0.17) |
0.18 (0.11–0.28) |
|
2 |
0.16 (0.03–0.79) |
0.48 (0.15–1.52) |
|
Bulky disease |
||
|
< 5 cm |
0.12 (0.06–0.24) |
0.23 (0.13–0.40) |
|
≥ 5 cm |
0.07 (0.02–0.19) |
0.14 (0.07–0.27) |
|
del(17)(p13.1) and/or TP53 mutation |
||
|
Yes |
0.10 (0.03–0.34) |
0.23 (0.09–0.61) |
|
No |
0.10 (0.05–0.18) |
0.19 (0.11–0.31) |
|
del(11)(q22.3) |
||
|
Yes |
0.09 (0.03–0.26) |
0.07 (0.02–0.22) |
|
No |
0.10 (0.05–0.20) |
0.26 (0.16–0.41) |
|
IGHV mutation status |
||
|
Unmutated |
0.08 (0.04–0.16) |
0.11 (0.07–0.19) |
|
Mutated |
0.15 (0.04–0.52) |
0.69 (0.31–1-56) |
Safety
The median duration of exposure was 27.7 months in Aca + O and Aca groups and 5.6 months in the Clb + O group. Frequent adverse events (AEs) of any grade, and Grade 3 or higher, reported across groups are summarized in Table 2.
Higher rates of serious AEs were reported with acalabrutinib-containing regimes (39%, and 32%, vs 22%), but that did not translate into a higher frequency of discontinuations due to AEs (11%, and 9%, vs 14%). The investigators associated this to the longer treatment duration, and consequently, to the greater exposure to acalabrutinib.
Table 2. Common AEs reported in at least 10% of patients in any treatment group.
|
Aca, acalabrutinib; AEs, adverse events; Clb, chlorambucil; O, obinutuzumab |
||||||
|
|
Aca + O |
Aca |
Clb + O |
|||
|---|---|---|---|---|---|---|
|
AEs, n (%) |
Any grade |
Grade ≥ 3 |
Any grade |
Grade ≥ 3 |
Any grade |
Grade ≥ 3 |
|
Headache |
71 (39.9) |
2 (1.1) |
66 (36.9) |
2 (1.1) |
20 (11.8) |
0 |
|
Diarrhea |
69 (38.8) |
8 (4.5) |
62 (34.6) |
1 (0.6) |
36 (21.3) |
3 (1.8) |
|
Neutropenia |
56 (31.5) |
53 (29.8) |
19 (10.6) |
17 (9.5) |
76 (45.0) |
70 (41.4) |
|
Fatigue |
50 (28.1) |
3 (1.7) |
33 (18.4) |
2 (1.1) |
29 (17.2) |
1 (0.6) |
|
Upper respiratory tract infection |
38 (21.3) |
4 (2.2) |
33 (18.4) |
0 |
14 (8.3) |
1 (0.6) |
|
Nausea |
36 (20.2) |
0 |
40 (22.3) |
0 |
53 (31.4) |
0 |
|
Infusion-related reactions |
24 (13.5) |
4 (2.2) |
0 |
0 |
67 (39.6) |
9 (5.3) |
|
Thrombocytopenia |
23 (12.9) |
15 (8.4) |
13 (7.3) |
5 (2.8) |
24 (14.2) |
20 (11.8) |
|
Anemia |
21 (11.8) |
10 (5.6) |
25 (14.0) |
12 (6.7) |
20 (11.8) |
12 (7.1) |
|
Pneumonia |
19 (10.7) |
10 (5.6) |
13 (7.3) |
4 (2.2) |
5 (3.0) |
3 (1.8) |
On the other hand, there were some predefined events of clinical interest related to cardiovascular AEs in the groups treated with the investigational drug. There were no major differences between groups in the incidence of atrial fibrillation and hypertension, but Grade ≥ 3 bleeding events occurred only in patients treated with acalabrutinib.
Ultimately, the authors did not identify any new safety signals in this trial, but noted that most AEs occurred within the first 6 months of treatment.
Discussion
This trial demonstrates the efficacy and safety of acalabrutinib, a selective Bruton’s Tyrosine Kinase inhibitor (BTKi), as first-line treatment for patients with CLL. In the reported interim analysis, receiving acalabrutinib ± obinutuzumab was associated with a statistically significant improvement of PFS over Clb + O.
Before the ELEVATE TN trial, there was no clear evidence in CLL of the added benefit of rituximab with a BTKi compared with conventional chemoimmunotherapy. In light of these results, the investigators emphasize the differences between rituximab and the third-generation CD20 antibody, obinutuzumab. When added to a BTKi, response rates were slightly better compared to the BTKi alone, and the authors hypothesize that with Aca + O combination, there is a higher probability of achieving not only a clinical response but also a deeper response. Undetected minimal residual disease rates in peripheral blood were higher in the Aca + O vs Aca group (49% vs 7% of patients with an investigator-assessed complete response).
However, this trial was not designed for comparison between the acalabrutinib-containing arms, and this should be further addressed in future studies, taking into account that some Grade 3 AEs were also more common in the Aca + O arm. Until then, it remains the physician's choice to add or not obinutuzumab according to the patient’s results and tolerability.
The median overall survival (OS) was not reached in any group, showing a need for a longer follow-up with continuous therapy to be able to analyze the long-term benefit of a non-chemotherapy regime as a first treatment option for CLL. By the time of this analysis, 79% of patients remained on therapy, and consequently, other secondary endpoints like time to next treatment, or PFS and OS comparison between Aca-arms will also need longer follow-up to be analyzed.
Nevertheless, the final analysis will face some limitations due to the study design: first of all, the differences in length of treatment period between arms; and second, the permitted crossover to acalabrutinib monotherapy of those patients progressing on Clb + O.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content

