All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The lym Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lym Hub cannot guarantee the accuracy of translated content. The lym and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lymphoma & CLL Hub is an independent medical education platform, sponsored by AbbVie, BeOne Medicines, Johnson & Johnson, Miltenyi Biomedicine, Nurix Therapeutics, Roche, Sobi and Thermo Fisher Scientific and supported through educational grants from Bristol Myers Squibb, Lilly and Pfizer. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lymphoma & CLL content recommended for you
Machine learning-based survival prediction models for advanced-stage Hodgkin lymphoma
Accurate prognostication is important for the optimal treatment selection in patients with classical Hodgkin lymphoma.1 The International Prognostic Score (IPS)-7 is typically used to risk-stratify patients with advanced-stage Hodgkin lymphoma (aHL).1 The IPS-3 model was developed to simplify the IPS-7 while retaining its predictive capabilities. Recently, the aHL International Prognostic Index (A-HIPI) was developed to improve prognostication compared with the IPS models.1
New predictive models developed using machine learning (ML) have the potential to further improve prognostication. Jørgensen et al.1 recently developed and validated an ML-based survival prediction model for patients with aHL and published the findings in Journal of Clinical Oncology Clinical Cancer Informatics. Below, we summarize the key points.
Methods and patient population1
- ML models were developed using data from adult patients with newly diagnosed aHL from the Danish National Lymphoma Register (development cohort).
- The model was validated using data from adult patients with newly diagnosed aHL from the Cancer Registry of Norway and the Swedish Lymphoma Register (validation cohort).
- Performance was measured by the integrated Brier score, the time-varying area under the curve (AUC), and the concordance index (C-index).
Key findings1
- In total, 1,467 patients were included (development cohort, n = 707; validation cohort, n = 760).
- Median follow-up was 7.2 years and 8.6 years in the development and validation cohorts, respectively.
- The ML model achieved the highest C-index for overall survival (OS) and progression-free survival (PFS) in both the development and validation cohorts (Table 1).
Table 1. Performance of the ML, IPS-3, IPS-7, and A-HIPI models in the development and validation cohorts*
|
Model |
Development cohort (n = 707) |
Validation cohort (n = 760) |
||||||
|
OS |
PFS |
OS |
PFS |
|||||
|
IBS |
C-index |
IBS |
C-index |
IBS |
C-index |
IBS |
C-index |
|
|
ML |
0.073 |
0.789 |
0.141 |
0.665 |
0.049 |
0.749 |
0.085 |
0.691 |
|
IPS-3 |
0.085 |
0.650 |
0.149 |
0.576 |
0.054 |
0.663 |
0.078 |
0.64 |
|
IPS-7 |
0.087 |
0.608 |
0.151 |
0.549 |
0.052 |
0.700 |
0.077 |
0.672 |
|
A-HIPI |
0.076 |
0.768 |
0.142 |
0.649 |
0.052 |
0.741 |
0.091 |
0.677 |
|
A-HIPI, advanced-stage Hodgkin lymphoma international prognostic index; C-index, concordance index; IBS, integrated Brier score; IPS, International Prognostic Score; ML, machine learning; OS, overall survival; PFS, progression-free survival. |
||||||||
- The time-varying AUC for OS and PFS was consistently higher for the ML model vs IPS-7 and IPS-3 in both cohorts.
- The time-varying AUC for the A-HIPI model was similar to the ML model for OS and PFS in the development cohort; this was similar for OS in the validation cohort.
- However, time-varying AUC for PFS was similar to the IPS-7 in the validation cohort.
- The 5-year OS and PFS rates for patients classified as high-risk by the ML and IPS-7 models are shown in Figure 1.
Figure 1. 5-year survival outcomes of high-risk patients in the ML model and IPS-7*
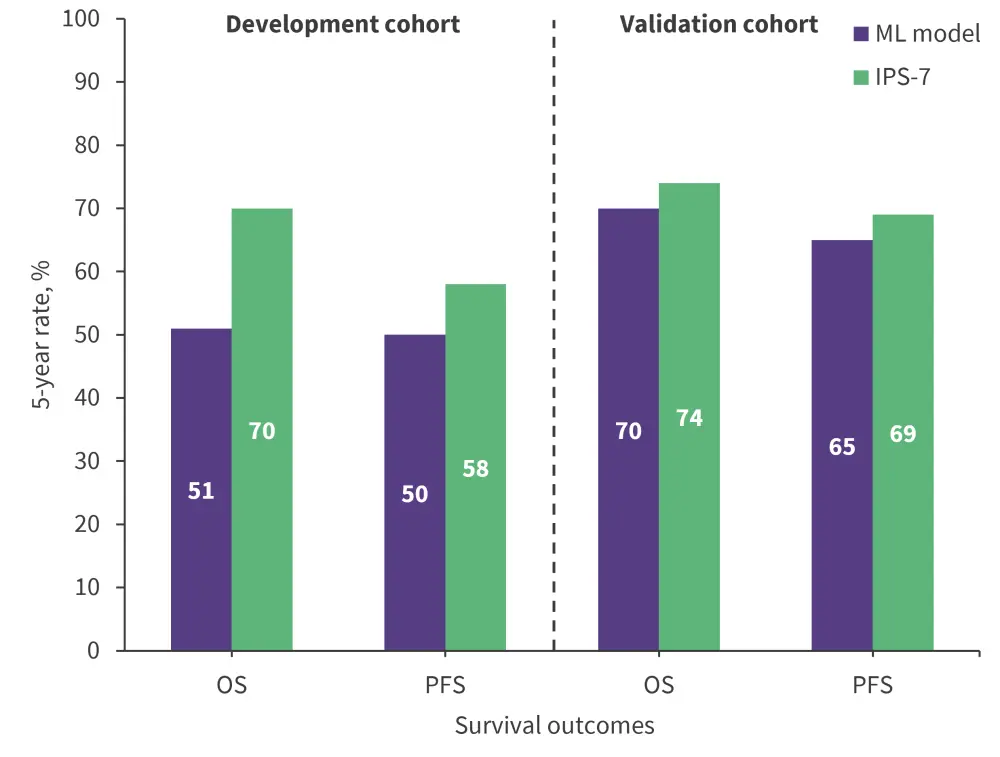
IPS, International Prognostic Score; ML, machine learning; OS, overall survival; PFS, progression-free survival.
*Data from Jørgensen, et al.1
| Key learnings |
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content


