All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The lym Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lym Hub cannot guarantee the accuracy of translated content. The lym and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lymphoma & CLL Hub is an independent medical education platform, sponsored by AbbVie, BeOne Medicines, Johnson & Johnson, Miltenyi Biomedicine, Nurix Therapeutics, Roche, Sobi, and Thermo Fisher Scientific and supported through educational grants from Bristol Myers Squibb, Lilly, and Pfizer. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lymphoma & CLL content recommended for you
The 5th edition of the World Health Organization classification of hematolymphoid tumors: T-cell lymphoma. Part 3
Do you know... Which of the following T-cell lymphomas is no longer considered a disease which only affects younger people?
The upcoming 5th edition of the World Health Organization (WHO) classification of hematolymphoid tumors (WHO-HAEM5) will reflect significant advances in the field since its last publication in 2017. This revised edition has systematically developed upon prior classifications and includes a restructuring of entities into a hierarchical system, updates to nomenclature, revision of diagnostic criteria or subtypes, deletion of certain entities, and introduction of new entities.
The Lymphoma Hub is pleased to present the third and final part in a series summarizing updates to the upcoming WHO-HAEM5, published on behalf of the WHO by Alaggio et al.1 in Leukemia. This final update is focused on T-cell lymphomas, highlighting changes since the revised 4th edition (WHO-HAEM4R). In our series, part one focused on updates and new additions to B-cell lymphoid proliferations and lymphomas, while part two was centered around diffuse large B-cell lymphoma.
Figure 1 and Figure 2 provide an overview of changes and new additions to the classification of T-cell lymphomas.
Figure 1. Changes to T-cell lymphomas classification*
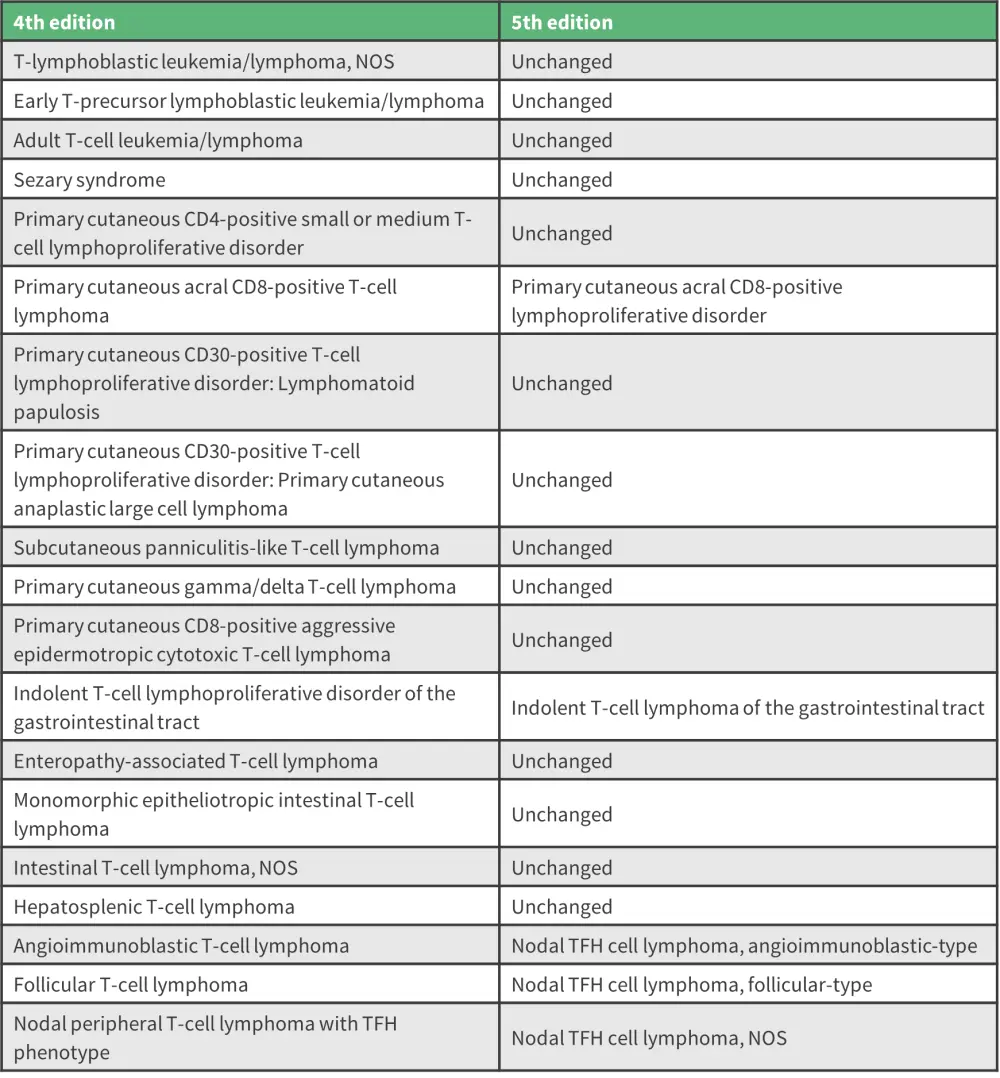
NOS, not otherwise specified; TFH, T-follicular helper.
*Adapted from Alaggio, et al.1
Figure 2. New additions to T-cell lymphoma category*
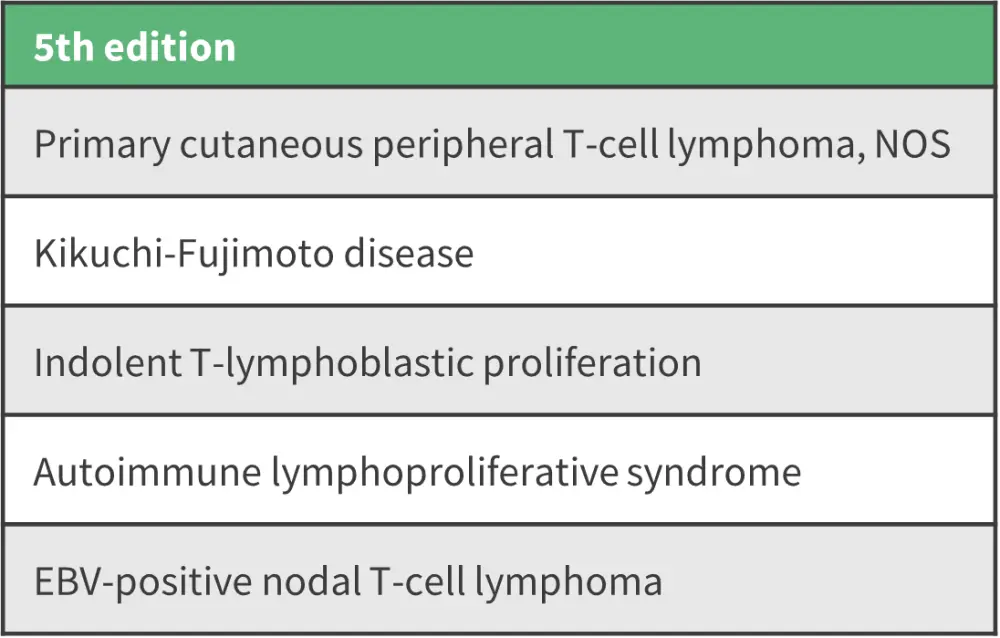
EBV, Epstein-Barr virus; NOS, not otherwise specified.
*Adapted from Alaggio, et al.1
Although most T-cell and natural killer (NK)-cell tumors can be classified according to their respective T- or NK-cell lineage, the WHO-HAEM5 does not divide them into two categories. This is due to some entities including a range of tumors with NK, T, hybrid, or indeterminate phenotypes, such as extranodal NK/T-cell lymphoma, Epstein-Barr virus positive nodal T- and NK-cell lymphoma, chronic active Epstein-Barr virus disease, and severe mosquito bite allergy.
Tumor-like lesions with T-cell predominance: new additions1
The WHO-HAEM5 includes three distinct entities: indolent T-lymphoblastic proliferation, Kikuchi-Fujimoto disease, and autoimmune lymphoproliferative syndrome, a new family of tumor-like lesions with T-cell predominance.
The expansion of T-cells may at times be mistaken for lymphoma. For example, indolent T-lymphoblastic proliferation is characterized by clusters of lymphoid cells ranging from small lymphocytes to larger cells with more open chromatin, like those observed in T-lymphoblastic lymphoma. Kikuchi-Fujimoto disease, which involves large aggregates and sheets of T immunoblasts and histiocytes accompanied by apoptosis in lymph nodes, mirrors peripheral T-cell lymphoma not otherwise specified (NOS). Autoimmune lymphoproliferative syndrome presents nodal infiltrates of CD4−, CD8− T cells which may appear as atypical medium-sized cells with clear cytoplasm, similar to those seen in lymphoma.
Primary cutaneous T-cell lymphoid proliferations and lymphomas: rare subtypes become entities
The WHO-HAEM4 included ‘cutaneous peripheral T-cell lymphoma, rare subtypes’, comprising primary cutaneous gamma/delta T-cell lymphoma, CD8-positive T-cell lymphoproliferative disorder, and CD4-positive small or medium T-cell lymphoproliferative disorder. However, in the WHO-HAEM5, these rare subtypes are listed as separate entities to recognize their specific clinicopathological and genetic characteristics.
The mycosis fungoides subtypes from WHO-HAEM4R still persist, but there have been changes to their classification. In the folliculotropic category, clinical early versus advanced stage patterns should be differentiated to recognize different clinical outcomes. Rare subtypes that do not fit other known cutaneous peripheral T-cell lymphomas are classed as a new group, “primary cutaneous peripheral T-cell lymphoma, NOS”. However, further studies are needed to understand their nature.
Intestinal T-cell and NK-cell lymphoid proliferations and lymphomas: indolent NK-cell lymphoproliferative disorder classification
‘Indolent T-cell lymphoproliferative disorder of the gastrointestinal (GI) tract’ has been renamed to ‘indolent T-cell lymphoma of the gastrointestinal tract’, and a new category called ‘indolent NK-cell lymphoproliferative disorder of the GI tract’ has also been added. The term ‘indolent T-cell lymphoma of the GI tract’ has been amended to reflect the significant morbidity caused by the tumor and its ability to spread.1 Research has shown interesting correlations between T-cell subsets and genetic changes in the neoplasm, including alterations in the JAK-STAT pathway.2
Indolent NK-cell lymphoproliferative disorder of the GI tract, previously thought to be a reactive process, has now been added as entity due to its neoplastic nature. Somatic mutations in genes, such as JAK3, and immunophenotypic features support a role for JAK3-STAT5 pathway activation in pathogenesis. There is a small percentage of patients who acquire new or persistent lesions from this benign condition, which often regresses within months.1
Hepatosplenic T-cell lymphoma: no longer confined to the young
In the WHO-HAEM5, this category has been refined due to recent evidence suggesting hepatosplenic T-cell lymphoma may not be limited to the younger population; one study reported only 49% of diagnosed patients were younger than 60 years of age.1
Nodal T-follicular helper cell lymphomas: new nomenclature to unite family members
Although the conceptual basis for recognizing nodal T-follicular helper cell lymphomas is consistent with those suggested in WHO-HAEM4R, WHO-HAEM5 introduces a common family name of ‘nodal T-follicular helper cell lymphomas’ (nTFHL), with previously recognized diseases regarded as entities within this family. This reflects the significant clinical and immunophenotypic likeness and plasticity. Therefore, the previously termed ‘lymphoma’, ‘follicular T-cell lymphoma’ and ‘peripheral T cell lymphoma with TFH phenotype’ have been renamed ‘nTFHL angioimmunoblastic-type’, ‘nTFHL follicular type’ and ‘nTFHL-NOS’, respectively. While research is required to provide further biological distinction between these entities, the current WHO-HAEM5 classification provides the basis for such developments.
Conclusion
Classification is subjective in nature and must be adaptable to change when new information becomes available. The WHO-HAEM5 has been updated to include new evidence as molecular complexity increases and diagnostic testing advances.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content



