All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The lym Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lym Hub cannot guarantee the accuracy of translated content. The lym and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lymphoma & CLL Hub is an independent medical education platform, sponsored by AbbVie, BeOne Medicines, Johnson & Johnson, Miltenyi Biomedicine, Nurix Therapeutics, Roche, Sobi, and Thermo Fisher Scientific and supported through educational grants from Bristol Myers Squibb, Lilly, and Pfizer. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lymphoma & CLL content recommended for you
CAPTIVATE 3-year update: fixed-duration ibrutinib + venetoclax in CLL/SLL
Ibrutinib, a Bruton’s tyrosine kinase inhibitor (BTKi) and venetoclax, a B-cell lymphoma 2 inhibitor, have distinct and complementary modes of action, targeting complementary cell compartments and chronic lymphocytic leukemia (CLL) subpopulations to eradicate both dividing and resting CLL cells. The primary analysis of the fixed-duration (FD) cohort of the phase II CAPTIVATE trial (NCT02910583) evaluating ibrutinib (I) in combination with venetoclax (V) as first-line therapy in patients with CLL/small lymphocytic lymphoma (SLL) has been previously summarized by the Lymphoma Hub. The primary analysis of the FD cohort has also recently been published by Tam, et al.,1 in Blood with an associated commentary by Rogers and Woyach.2 These results demonstrated durable response and a favorable safety profile with FD I + V treatment. The primary analysis also showed that patients with unmutated immunoglobulin heavy chain variable had higher likelihood of undetectable minimal residual disease (uMRD). However, these findings called for longer follow-up to examine if the negative impact of unmutated immunoglobulin heavy chain variable on progression-free survival (PFS) is reversed using this combination, and if inclusion of a BTKi mitigates the effect of del(17p). At the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting, the 3-year follow-up data of the FD cohort from the CAPTIVATE trial was reported by William G. Wierda.3 The key updates are summarized below.
Study design
The CAPTIVATE FD cohort included patients aged ≤70 years with previously untreated CLL/SLL, requiring treatment according to International Workshop on Chronic Lymphocytic Leukemia 2008 criteria with an Eastern Cooperative Oncology Group Performance Status of 0–2. The treatment schedule is shown in Figure 1.
Figure 1. Treatment schedule*
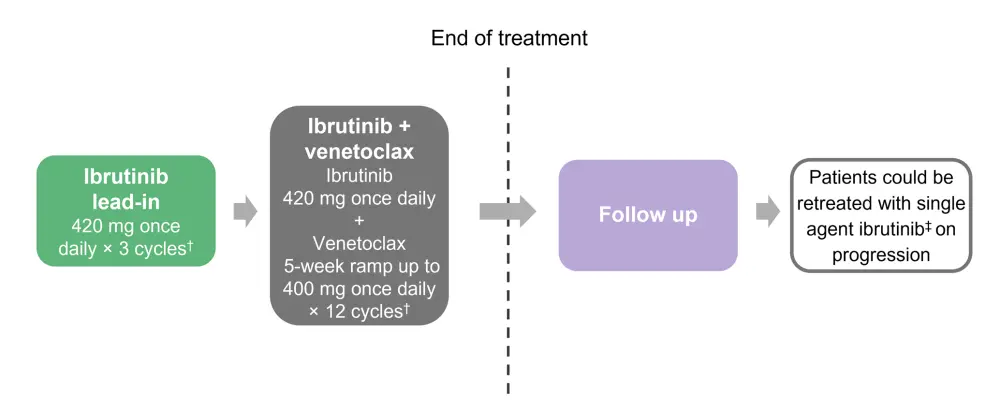
FD, fixed duration
*Adapted from Wierda.3
†Each cycle was 28 days.
‡Or FD ibrutinib + venetoclax if they had durable response.
The primary endpoint was investigator assessed complete response (CR) rate including complete response with incomplete hematologic recovery in patients without del(17p). Secondary endpoints included undetectable overall response rate, duration of response, uMRD rates (10-4 by flow cytometry), PFS, overall survival (OS), reduction in tumor lysis syndrome (TLS) risk category, and safety.
Results
A total of 159 patients were included, of which 92% completed the treatment.
Efficacy
With an additional year of follow-up since the primary analysis reported in 2021 (median duration of follow-up, 38.7 months; range, 0.8–41.1 months), the overall response rate was 96%; consistent in patients who had high-risk features. The median duration of treatment was 13.8 months. The PFS and OS at 36 months were 88% and 98%, respectively, and remained consistent in patients with high-risk features (Table 1).
In the FD cohort, 16 patients from the time of primary analysis and ten new patients from the additional 1-year follow-up had progressive disease. Of these, 22 patients had no BTK, PCLy2 or BCL-2 mutations associated with resistance to ibrutinib or venetoclax.
Table 1. Efficacy outcomes*
|
CR, complete response; CI, confidence interval; FD, fixed duration; ORR, overall response rate; OS, overall survival; PFS, progression-free survival; uIgHV, unmutated immunoglobulin heavy chain variable. |
|||
|
Efficacy outcomes, % |
FD cohort† |
del(17p)/TP53 |
uIgHV |
|---|---|---|---|
|
ORR |
96 |
96 |
97 |
|
CR‡ |
57 |
56 |
64 |
|
PFS at 36 months |
88 (82–92) |
80 (58–91) |
86 (77–92) |
|
OS at 36 months |
98 |
96 |
97 |
At a median duration of 25 months after completion of treatment, FD I + V continued to provide deep and durable responses. The CR rate showed a nominal increase at the additional one-year follow-up compared with the primary analysis (57% vs 55%) in all patients, and similar results were observed in patients without del(17p) (Figure 2). Median duration of CR and duration of response has not yet been reached.
Figure 2. Best ORR to FD treatment with I + V*
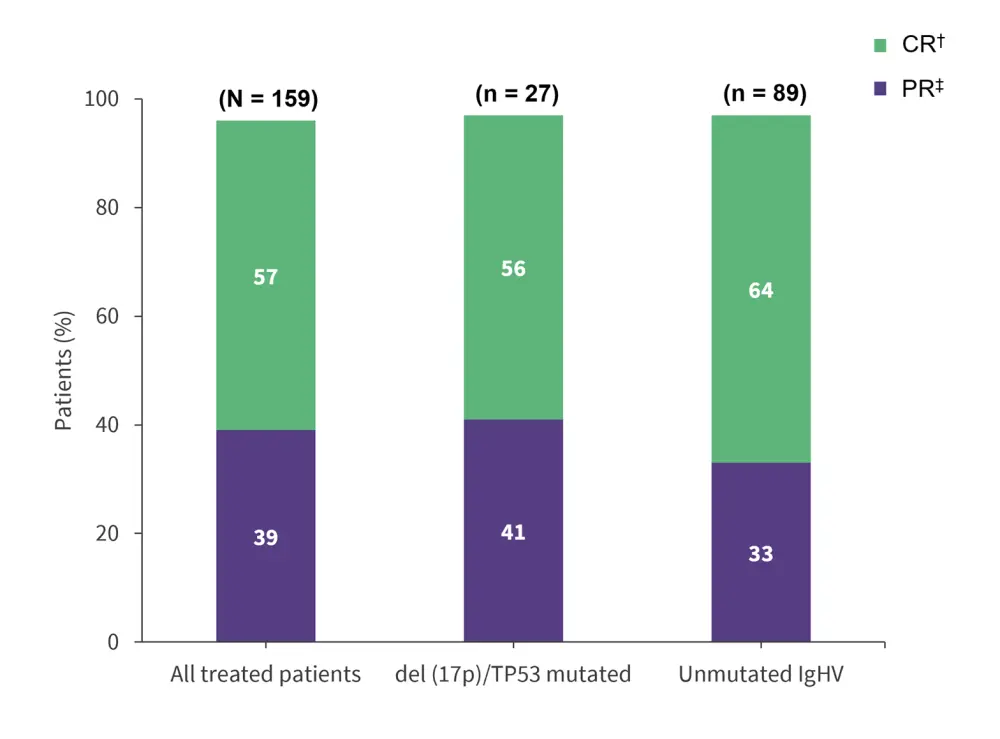
CR, complete response; FD, fixed duration; I, ibrutinib; IgHV, immunoglobulin heavy chain variable; ORR, overall response rate; PR, partial response; V, venetoclax.
*Adapted from Wierda.3
†Includes nodular PR.
‡Includes patients achieving complete response with incomplete hematologic recovery.
Overall, 79% (125/159) of patients achieved uMRD in peripheral blood and/or bone marrow. Among patients who achieved uMRD in peripheral blood at Month 3 posttreatment, 78% maintained uMRD to Month 12.
Figure 3. Post-treatment blood uMRD*
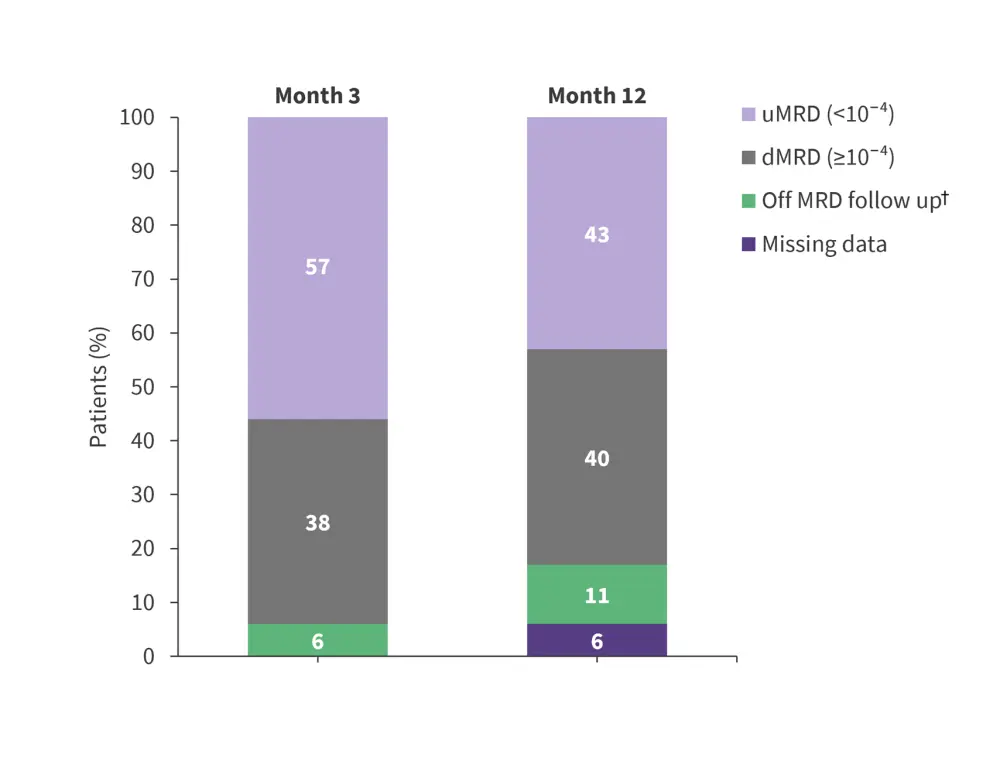
d, detectable; MRD, minimal residual disease; u, undetectable.
*Adapted from Wierda.3
†Included patients who met any one of the criteria: progressive disease, initiation of subsequent therapy, death, or withdrawal from the study.
Safety
Following three cycles of ibrutinib lead-in, patients with a high tumour burden category [MM1] for TLS reduced from 21% to 1% compared with baseline, and patients needing hospitalization for TLS monitoring decreased from 40% to 18%.
The most frequent treatment-emergent adverse events were Grade 1 and 2, except for neutropenia (Figure 4). The median time to onset for frequently occurring treatment-emergent adverse events was within 4 months and median time to resolution or improvement ranged from 16.5–42.5 days[MM2] . One fatal adverse event (AE) occurred during ibrutinib lead-in, but no serious AEs were reported at the additional 1-year follow-up; the safety profile remained unchanged as previously reported.
Among AEs of clinical interest, atrial fibrillation of any grade and Grade ≥3 occurred in 4% and 1%, respectively, and major haemorrhage in 2% of patients.
Figure 4. Frequently occurring TEAEs*
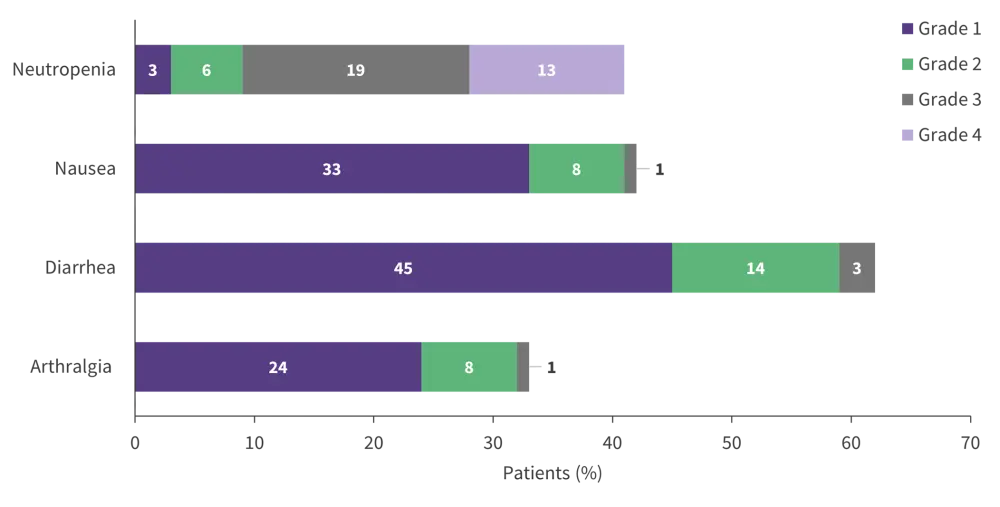
TEAEs, treatment-emergent adverse events.
*Adapted from Wierda.3
With regards to retreatment, 12 patients progressed after FD I + V treatment and were treated with single-agent ibrutinib for between 6–32 months. Of these, 11 patients were evaluable for response, with nine patients achieving partial response with rebound lymphocytosis and one achieving stable disease.
Conclusion
The 3-year follow-up of the FD cohort showed that I + V continues to demonstrate deep and durable responses, with a clinically meaningful PFS rate of 88% which included patients with high-risk features such as TP53 abnormalities. There were no OS events at the additional 1-year follow up and the manageable safety profile was consistent with the primary analysis. These findings suggest that I + V offers an efficacious, chemotherapy-free, oral FD regimen that can be delivered in the outpatient setting for most young and fit patients with CLL or SLL. Early data also suggests that patients who progressed after FD I + V treatment can be successfully retreated with single-agent ibrutinib. However, the findings may not be applicable to the overall population of patients with CLL who tend to be older with comorbidities. Inclusion of oral venetoclax in the regimen reduced infusion visits; however, outpatient visits were needed to start the regimen which poses a challenge for some patients and clinics, future trials should consider this.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content




