All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the Lymphoma Coalition.
The lym Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the lym Hub cannot guarantee the accuracy of translated content. The lym and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Lymphoma & CLL Hub is an independent medical education platform, sponsored by AbbVie, BeOne Medicines, Johnson & Johnson, Miltenyi Biomedicine, Nurix Therapeutics, Roche, Sobi, and Thermo Fisher Scientific and supported through educational grants from Bristol Myers Squibb, Lilly, and Pfizer. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View lymphoma & CLL content recommended for you
Efficacy and safety of ibrutinib + BR in the treatment of elderly patients with MCL: Primary analysis from SHINE III
Mantle cell lymphoma (MCL) is a rare B-cell non-Hodgkin lymphoma, it is known to have an aggressive disease course and continues to be a clinical challenge due to its incurability with existing therapies, presenting a significant unmet clinical need. Many patients with MCL are older and unsuitable for intense treatment options, including autologous hematopoietic stem cell transplantation. However, the treatment landscape for MCL has been transformed with ibrutinib, an oral Bruton’s tyrosine kinase inhibitor (BTKi), which has shown durable activity in patients with relapsed/refractory (R/R) MCL.
During the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting, Michael Wang presented preliminary results from the phase III SHINE trial (NCT01776840) evaluating the efficacy and safety of ibrutinib in combination with bendamustine-rituximab (BR) and rituximab maintenance in elderly patients with MCL.1 Below, we summarize the key findings, which have also been recently published in The New England Journal of Medicine.2
Study design
This is a double-blind, placebo-controlled, phase III randomized trial in elderly patients aged ≥65 years with stage II–IV disease and previously untreated MCL. Patients were either randomized to ibrutinib + BR or placebo + BR arms (Figure 1).
The primary endpoint was investigator assessed progression free survival (PFS). Secondary endpoints included overall response rate, time to next treatment, overall survival (OS), and treatment emergent adverse events (TEAEs).
Figure 1. Treatment schema*
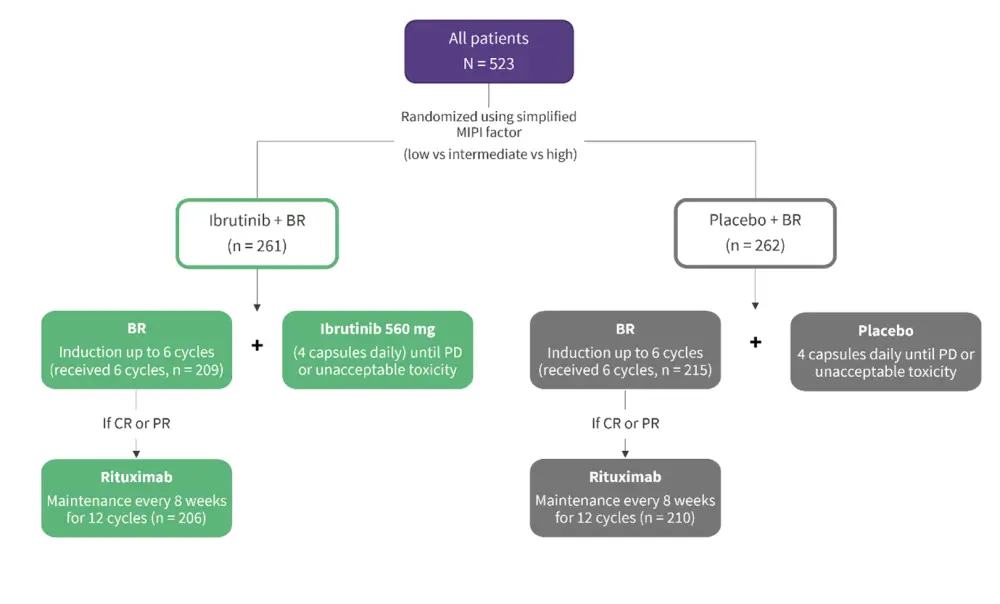
BR, bendamustine-rituximab; CR, complete response; MIPI, Mantle Cell Lymphoma International Prognostic Index; PD, progressive disease; PR, partial response.
*Adapted from Wang.1
Results
Baseline characteristics
A total of 523 patients were included with a median age of 71 years (range, 65–87 years; Table 1). The median duration of placebo exposure was longer compared with ibrutinib (34.1 vs 24.1 months, respectively). The most common reason for discontinuation of treatment was adverse events (n = 103) and progressive disease (n = 91) in the ibrutinib + BR and placebo + BR arms, respectively.
Table 1. Baseline characteristics*
|
BM, bone marrow; BR, bendamustine-rituximab; ECOG, Eastern Cooperative Oncology Group; MIPI, Mantle Cell Lymphoma International Prognostic Index. |
||
|
Characteristics, % (unless otherwise stated) |
Ibrutinib + BR |
Placebo + BR |
|---|---|---|
|
Age |
||
|
Median age (range), years |
71 (65–86) |
71 (65–87) |
|
≥75 years |
28.4 |
31.3 |
|
Male |
68.2 |
71.0 |
|
ECOG Performance Status 1 |
48.7 |
45.0 |
|
Simplified MIPI score |
||
|
Low risk |
16.9 |
17.6 |
|
Intermediate risk |
47.5 |
49.2 |
|
High risk |
35.6 |
33.2 |
|
BM involvement |
75.9 |
76.3 |
|
Blastoid/pleomorphic histology |
7.3 |
9.9 |
|
Extranodal |
89.7 |
86.3 |
|
Bulky (≥5 cm) |
36.4 |
37.4 |
|
TP53 mutated |
10 |
9.2 |
PFS
As of the data cut-off (June 2021), the primary endpoint of PFS was met with a median follow-up of 85.1 months. Patients in the ibrutinib + BR arm showed a significant improvement in the median PFS compared to placebo + BR arm (80.6 vs 52.9 months; hazard ratio [HR], 0.75; p = 0.011). The longer median PFS demonstrated by ibrutinib + BR compared to placebo + BR (6.7 vs 4.4 years) equated to an additional 2.3 years of PFS. All except patients in the high-risk group showed improved in PFS with ibrutinib + BR (Table 2). Patients in the high-risk group with blastoid/pleomorphic histology had a median PFS of 25.6 vs 10.3 months (HR, 0.66); those with TP53 mutation had a median PFS of 28.8 vs 11 months (HR, 0.95) in the ibrutinib + BR and placebo + BR arms, respectively.
Table 2. PFS hazard ratios by subgroup*
|
BR, bendamustine-rituximab; CI, confidence interval; ECOG, Eastern Cooperative Oncology Group; MIPI, Mantle Cell Lymphoma International Prognostic Index. |
||||
|
Characteristics, n/N |
Ibrutinib + BR |
Placebo + BR |
Hazard ratio |
95% CI |
|---|---|---|---|---|
|
Sex |
||||
|
Male |
88/178 |
111/186 |
0.77 |
0.58–1.02 |
|
Female |
28/83 |
41/76 |
0.65 |
0.40–1.06 |
|
Race |
||||
|
White |
92/199 |
118/206 |
0.78 |
0.60–1.03 |
|
Non-white |
24/62 |
34/56 |
0.59 |
0.35–1.00 |
|
Age |
||||
|
<70 years |
39/99 |
62/108 |
0.67 |
0.45–0.99 |
|
≥70 years |
77/162 |
90/154 |
0.78 |
0.58–1.06 |
|
ECOG Performance Status |
||||
|
0 |
53/134 |
72/141 |
0.69 |
0.49–0.99 |
|
1–2 |
63/127 |
80/121 |
0.77 |
0.56–1.08 |
|
Simplified MIPI score |
||||
|
Low risk (0–3) |
15/44 |
21/46 |
0.85 |
0.44–1.65 |
|
Intermediate risk (4–5) |
42/124 |
76/129 |
0.50 |
0.34–0.73 |
|
Low intermediate risk (0-5) |
57/168 |
97/175 |
0.57 |
0.41–0.78 |
|
High risk (6–11) |
59/93 |
55/87 |
1.02 |
0.71–1.48 |
|
Tumor bulk |
||||
|
<5 cm |
64/165 |
90/163 |
0.71 |
0.51–0.97 |
|
≥5 cm |
51/95 |
62/98 |
0.78 |
0.54–1.13 |
Other key outcomes
The overall response rate was 89.7% in the ibrutinib + BR and 88.5% in the placebo + BR arm. The complete response rate was higher in the ibrutinib + BR compared with placebo + BR arm (65.5% vs 57.6%; p = 0.057).
Time to next treatment has yet not been reached by patients in the ibrutinib + BR arm compared to a median of 92 months in the placebo + BR arm (HR, 0.48). Subsequent therapies at second line were needed by 19.9% vs 40.5% of patients in the ibrutinib + BR and placebo + BR arms, respectively. Of note, 38.7% of patients in the placebo + BR arm received a BTKi as subsequent therapy.
The most common TEAEs of any grade included neutropenia (51.4%), diarrhea (46.3%), and nausea (41.3%) in the ibrutinib + BR arm. The occurrence of rash and pneumonia was higher in the ibrutinib + BR arm (33.6% vs 23.5%) and showed a higher frequency of any bleeding and atrial fibrillation compared to placebo + BR arm (Table 3). Secondary primary malignancies occurred 21% and 19% of ibrutinib + BR and placebo + BR arm patients, respectively.
Median OS has not yet been reached in both ibrutinib + BR and placebo + BR arms (HR, 1.07) and the data on OS will continue to develop as the trial progresses. At data cut-off, a total of 211 patients had died, including five patients who had died due to Covid-19. Deaths due to progressive disease (20.6% vs 11.5%) were higher and deaths due to TEAEs (6.1% vs 10.7%) were lower in the placebo + BR arm compared with those in the ibrutinib + BR arm.
Table 3. TEAEs of clinical interest with BTKi*
|
BR, bendamustine + rituximab; BTKi, Bruton’s tyrosine kinase inhibitor; TEAE, treatment-emergent adverse event. |
||||
|
|
Ibrutinib + BR (n = 259) |
Placebo + BR (n = 260) |
||
|---|---|---|---|---|
|
TEAE, % |
Any grade |
Grade 3 or 4 |
Any grade |
Grade 3 or 4 |
|
Any bleeding† |
42.9 |
3.5 |
21.5 |
1.5 |
|
Major bleeding† |
5.8 |
— |
4.2 |
— |
|
Atrial fibrillation |
13.9 |
3.9 |
6.5 |
0.8 |
|
Hypertension |
13.5 |
8.5 |
11.2 |
5.8 |
|
Arthralgia |
17.4 |
1.2 |
16.9 |
0 |
Conclusion
The primary analysis of the ongoing phase III SHINE trial shows that ibrutinib + BR significantly improved PFS in elderly patients with untreated MCL compared with other chemoimmunotherapy. Ibrutinib + BR achieved a clinically meaningful 2.3-year PFS advantage compared with placebo + BR. The trial also shows that the safety profile of ibrutinib is consistent with the existing profiles of the individual drugs. However, adverse events such as pneumonia, bleeding, and atrial fibrillation were higher in the ibrutinib + BR arm. In the context of increased toxicity, approaches to time-limited use of ibrutinib and in selected subset of patients with MCL needs further exploration. The authors concluded that these findings should set a new benchmark for first-line therapy, both in older patients with MCL and those not eligible for autologous hematopoietic stem cell transplantation.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content



